Case of the month – March

We present the case of a 3 years old girl, referred to our clinic for failure to thrive, eating difficulties and chronic diarrhea.
She comes from non-consanguineous parents, but with a sister deceased at the age of 6 months, of unknown cause.
She was diagnosed before age 1 with cow’s milk allergy and started the cow’s milk protein exclusion diet. Early gluten introduction was noted.
At the age of 1 year and 3 months she was diagnosed with celiac disease based on strong clinical presumption and positive antigliadin antibodies. The clinical presentation was highly compatible with malnutrition, due to severe malabsorption syndrome, celiac crisis. The gluten-free diet was started, without performing intestinal biopsy or measuring tTG-ab and/or EMA.
She was later reffered to our centre for follow-up. During follow-up examinations, it was noticed that, in fact, her growth hadn’t improved much with the gluten-free diet, as seen below. Signs and symptoms of malabsorption were still present.
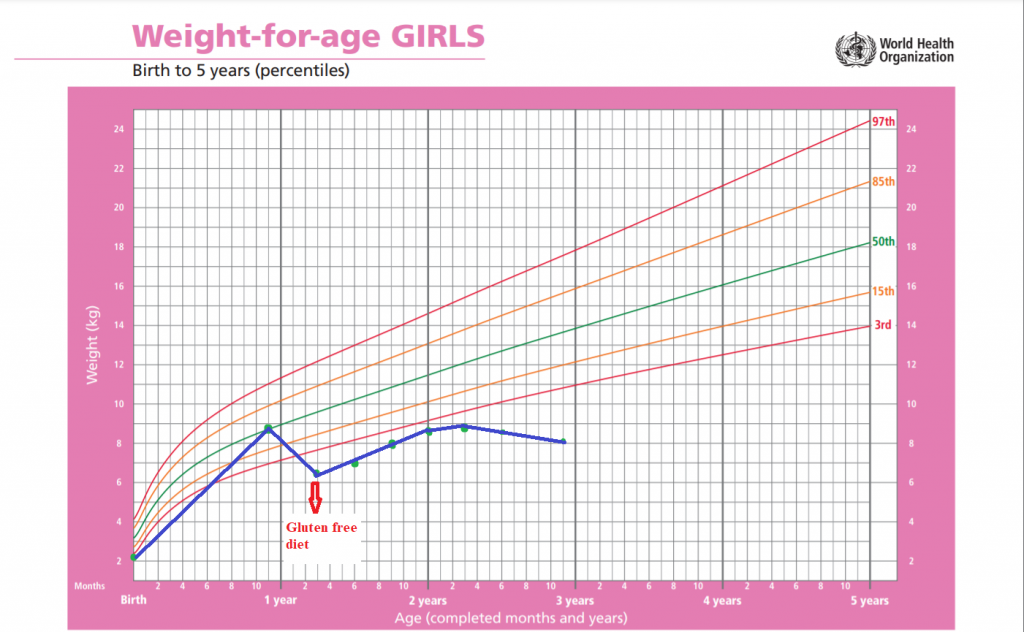
Clinically : her weight was 8 kg, with signs of malnutrition, and diarrhoea. Particular facial and body features such as widened base of the nose, tall forehead, hypertelorism, woolly hair and 10 cafe-au-lait spots of various dimensions spread across the body were also noticed after clinical examination. Further evaluations showed also cognitive retardation.
She was referred to our genetician, who confirmed the presumption of a genetic disorder, and opted for a Whole Exome Sequencing (WES), which found TTC37 mutation known to cause the Trichohepatoenteric syndrome.
The syndrome consists of three main features: hair modifications, hepatic disfunction and intractable diarrhoea. Other signs and symptoms include unusual facial appearance, immunodeficiency traits and mental retardation.
The treatment consists of symptomatic therapies such as nutritional therapy. In some cases iv immunoglobulins are used, when clear immunodeficiencies are associateid. In severe cases, such as liver cirrhosis, liver transplant is indicated.
In roughly 50% of the cases, the children don’t survive childhood, due to the hepatic illness or immunodeficiency.
Discussion : the severe clinical picture in this case together with the antigliadin antibodies (used to be regarded as an evaluation tool in children younger than 2 years of age, according to earlier guidelines) led in this case to a « fast track » decision towards celiac disease diagnosis. The treatment (gluten-free diet) failure, with basically no improvement, was the main trigger for the reevaluation. In this particular case, most probably the intestinal biopsy, if done, would have shown some degree of villous atrophy with/without increased IELs, but could have been missleading also.
The child will be put on a gluten challenge with follow-up testing, but the presence of celiac disease in this case seems unlikely, or, in any case, not the main determinant of the clinical picture, outcome and long term prognosis.
Conclusion : the diagnosis of celiac disease is sometimes challenging, therefore it is recommended to follow the current guidelines and moreover, try to obtain as much information as possible BEFORE starting the gluten-free diet. In this case, the follow-up was critical for the reconsideration of the diagnosis.