Discovery of genetic association in a CD diagnosed patient

We present the case of a 41 years old female, who was diagnosed with Celiac Disease at the age of 9. At the time she presented with recurrent aphthous stomatitis, short stature (<5th percentile) and iron-deficient anemia. The clinical presentation oriented to an atypical form of CD, that was confirmed by intestinal biopsy, showing severe mucosal lesions with total villous atrophy.
Clinically she also had a peculiar phenotype, short-stature, micrognathia, low-set ears, low posterior hairline and short fingers, that oriented to a Turner’s syndrome, but the genetic tests performed could not confirm the diagnosis.
After discharge, the patient failed to attend the out-patient appointments. She was recalled 18 years later, on the occasion of a recall of all celiac patients diagnosed in the clinic, and she responded to the invitation. At presentation, she had a short stature (<5th percentile), overweight (58 kg), poor hearing, cutaneous erythematous plaques lesions on eyelids and elbows, short fingers, poor secondary sexual characteristics (low breast development, amenorrhea) and recurrent abdominal pain. She was on a low gluten containing diet. The cutaneous lesions showed clinical improvement during complete gluten-free diet.
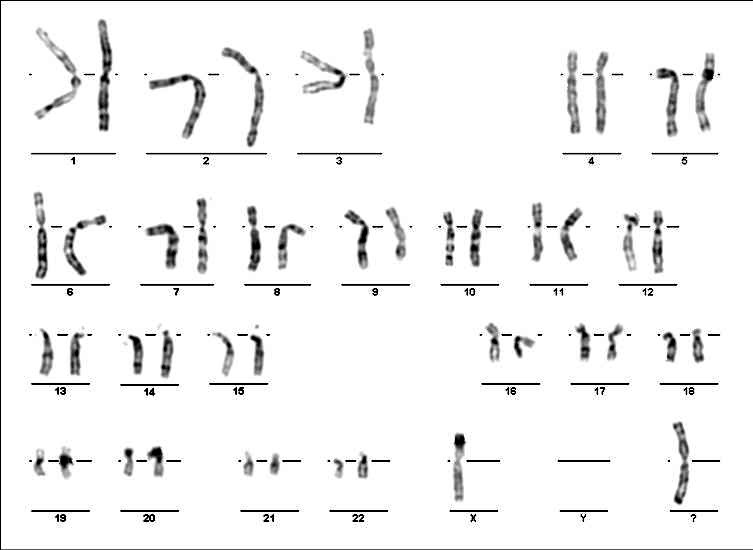
Genetic tests were taken, and this time, with the help of new methods (peripheral lymphocyte karyotype), the diagnosis could be made. It was a Turner’s syndrome variant 46Xi (Xq).
The laboratory findings showed high FSH level, positive markers of CD (high titers of specific antibodies) and indirect signs of malabsorption (low proteinemia, low cholesterol, iron-deficient anemia).
The abdominal ultrasound revealed small ovaries, with polycystic appearance. No cardiac or renal abnormality were found.
She was also diagnosed with bilateral sensorineural and conductive hearing loss. Intellectual performance was normal.
The karyotype analysis of our patient reveals the most common structural abnormality in Turner’s Syndrome, associated with autoimmune disorders and deafness. (see figure at the end)
Our patient developed at least one autoimmune disorder (celiac disease) and progressive hearing loss. It is not clear whether the cutaneous lesions represent a second autoimmune disorder (psoriasis) or cutaneous manifestations of celiac disease (dermatitis herpetiformis). The peculiar disposition on the face and the disappearance during the gluten-free diet compliance periods could be a reason to sustain a celiac disease symptom.
In our case the failure of the follow-up system caused the poor compliance on the gluten-free diet and the delay of the genetic diagnosis.
These patients need a variety of follow-up controls: repeated serologic tests for celiac disease activity, echocardiography, hearing aid controls, endocrinological assessment, sex hormone replacement therapy.
The patient had a poor outcome in the absence of GFD and adequate endocrinological treatment, needing sustained, long-term follow-up by a multidisciplinary team.
14 years later, back to our days, the patient is using a hearing device, she is following a strict gluten-free diet for her CD, and a hormonal therapy for her Turner’s syndrome, she has no more skin lesions or gastro-intestinal symptoms, her speech improved a lot, she finished universitary studies, had a PhD abroad and she is now teaching at an engineering university in Bucharest.